Islets of Langerhans (Beta Islet Cells)
** Definition, Histology, Function, and Location
Definition
Also known as the islands of Langerhans, the Islets of Langerhans is an endocrine tissue located within the pancreas (below the liver and behind the stomach). It consists of a variety of cells capable of producing different hormones that are then released into the bloodstream to be transported to their respective target sites.
One of the main groups of cells within the Islets of Langerhans, and the subject of this article, are beta islet cells. These cells play a central role in the production, storage, and release of a peptide hormone known as insulin in animals.
The other cells located within the Islets of Langerhans include:
· Alpha cells - Involved in the production of glucagon
· Pancreatic polypeptide cells (PP cells) - Produce pancreatic polypeptide
· Delta cells - Involved in the production of somatostatin
· Episilon cells - Involved in the production of ghrelin (a gut hormone)
* Beta make up between 64 and 80 percent of the total cells in the islets of Langerhans.
* The islets of Langerhans makes up about 1% of the entire pancreas.
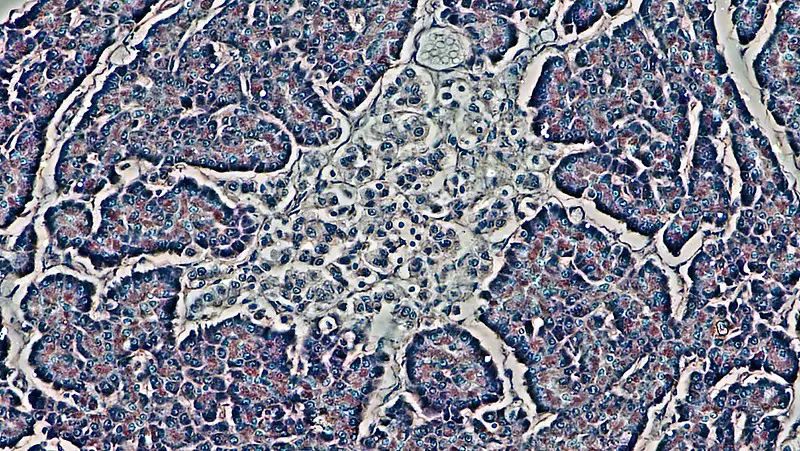
Histology
A number of techniques have been used to identify and distinguish between the different types of cells in the Islets of Langerhans.
These include:
· Chromium Hematoxylin-phloxine Method
· Aldehyde Fuchsin Method
· Barrnett and Seligman Technique
· Zinc and Cobalt Techniques
Gomori's Chromic Hematoxylin-Ponceau Staining Technique
While there are a number of available techniques, this section will focus on the Gomori's Chromic Hematoxylin-Ponceau method. One of the biggest advantages of this approach is the fact that it makes it possible to clearly distinguish Beta cells from the other types of cells in the Islets of Langerhans.
Procedure
· For this technique, a sample from a rabbit or rat can be used
· A section from the sample is first treated with potassium permanganate for about 2 minutes (Potassium permanganate from Gomori's formula)
· Wash the section in running tap water - 1 minute
· Bleach section with 5% potassium meta-bisulfite - 1 minute
· Wash section in running tap water - 5 minutes
· Stain the section using chromic hematoxylin - 30 minutes at room temperature (about 10 minutes at 52-65°C)
· Rinse section in 95% alcohol - Until color washes out completely
· Immerse in 1% solution of reagent HCL in 95 percent alcohol to differentiate - 1 minute
· Wash the section with tap water - 5 to 10 minutes
· Stain the section using ponceau-fuchsin - 15 to 45 minutes
· Rinse the section in 1% acetic acid
· Immerse in 1% phosphomolybdic acid - 5 to 30 minutes to differentiate
· Rinse the section in 1% acetic acid two times - 1 minute
· Dehydrate and mount the section to observe under the microscope
Results
When viewed under the microscope, Alpha islet cells will appear deep red in color while Beta cells appear deep blue or black. Granules of Beta cells stain steel blue to black in color.
Here, it's also possible to identify pale red spots within the Beta cells given that the mitochondria stain pale red in color (the cytoplasm are pale gray).
Results for the other cells:
· Cytoplasm of Delta cells will gray to gray-orange in color
· Mitochondria of Delta cells will appear pale to orange-red in color
· Granules of Delta cells stain deep blue
Islets of Langerhans General Characteristics
Depending on the age of the person or type of animal the Islets of Langerhans measures between 50 to 300 micrometers in size. As mentioned, Beta cells are the most prevalent cells in this tissue, making up about 70% of all cells.
When viewed under the microscope (under strong magnification), they are usually surrounded by Alpha cells and the other types of Islet cells. Compared to Alpha and Delta cells, Beta cells are generally smaller in size.
They have all been shown to communicate with each other through various extracellular materials and gap junctions. This allows products produced by one type of cell to influence the activity/response of the other cells.
Surrounded by the other cells, Alpha cells being the most abundant, the Beta cells are clustered close together. Using a scanning and transmission electron microscope, they were shown to be round or oval in shape, measuring about 10 microns in diameter.
In some studies involving mice, it has been shown that Beta cells resemble truncated pyramids allowing them to be packed close together in a cluster.
* Like other cells, Beta cells also contain a number of important organelles including ribosomes and the mitochondria.
Insulin granules are also prevalent, visible under electron microscope, and measure about 300 nanometers in diameter. There are an estimated 10,000 insulin granules in each Beta cell.
Functions
Insulin Synthesis
Beta cells of the Islets of Langerhans are primarily involved in the production of insulin. In animals, this is an important hormone that is released into the bloodstream in order to influence sugar uptake (thus reducing the sugar level in the blood).
In the Islets of Langerhans, Alpha cells are involved in the production of glucagon; the hormone that raises blood sugar levels by influencing the conversion of glycogen to glucose in the liver.
Under normal circumstances, the blood sugar level is between 80 and 120 mg/dl. Blood sugar level above this in the body is known as hyperglycemia and can result in a number of symptoms related to diabetes.
* Insulin synthesis in Beta islet cells starts in the ribosome. Here, information from mRNA is translated by ribosomes to produce preproinsulin at the rough endoplasmic reticulum. This molecule (pre-proinsulin) is then cleaved by a peptidase enzyme in the endoplasmic reticulum to produce proinsulin.
From the endoplasmic reticulum, proinsulin is transported to the Golgi body for packaging (into secretory vesicles/granules). Within the vesicles, proinsulin is again cleaved into insulin and C-peptide.
Insulin in the Liver Cells
Glucose that enters the Beta cells from blood undergoes glycolysis and the Kleb cycle to produce NADH and FADH2 which are used in the mitochondria to produce ATP energy. The ATP binds to the potassium channel on the membrane of the Beta cell causing it to close.
As a result, there is an accumulation of potassium ions within the cell which causes the membrane potential to become highly positively charged. This stimulates the calcium channels to open and allow calcium ions into the cell.
In the cell, calcium causes the membrane of vesicles storing insulin to fuse with the membrane of the cell thus allowing insulin to be released into the blood. From the blood, insulin moves to the liver where it stimulates the conversion of glucose to glycogen.
* In the liver, insulin binds to tyrosine kinase receptors located on the surface of the liver cells. This results in the production of PI3K and AKT. As glucose enters the cells of the liver through GLUT2 (glucose transporter), it's converted to glycogen through the actions of the two enzymes. This process is known as glycogenesis.
* By influencing the activities of glycolytic enzymes, insulin also stimulates the conversion of glucose to pyruvate within the liver. Pyruvate then goes through glycolysis ultimately resulting in the production of ATP.
Insulin in Muscle Cells
From the blood, insulin also moves to the muscle cells where it binds to tyrosine kinase receptors. Like in the liver cells, insulin also activates the production of Phosphoinositide 3-kinase and Protein kinase B (PI3K/AKT).
In turn, these proteins activate GLUT4 (an insulin-dependent glucose transporter) to become more active and take in more glucose molecules.
In these cells, the two proteins (PI3K/AKT) again stimulate glycolysis where glucose is first converted to pyruvate and then used to produce ATP. PI3K/AKT also stimulates the uptake of more amino acids through the amino acid channels for protein synthesis (amino acids are used to make proteins).
* In muscle cells, insulin also stimulates the conversion of glucose to glycogen through the actions of PI3K/AKT.
Insulin in the Cells of Adipose Tissue
In adipose tissue, insulin also binds to the cell receptors and stimulates the production of PI3K/AKT. As is the case in muscle cells, PI3K/AKT activates GLUT4 transporters causing them to become hyperactive. This results in increased uptake of glucose into the adipose cells.
Here, the glucose is broken down into Dihydroxyacetone phosphate and Glyceraldehyde 3-phosphate which are then converted into glycerol and fatty acids respectively (under the influence of PI3K/AKT). The two molecules are then combined to produce triacylglyceride (TAG). This process is known as lipogenesis.
* In the liver, muscles, and adipose tissue, insulin promotes the uptake of sugar/glucose (and amino acids) from blood so that it can be transformed into other molecules (ATP, TAG, glycogen, etc.) that can be stored. In doing so, the sugar level in blood is reduced to ensure that it's back to normal.
However, in the event of low blood sugar, glucagon is released by Alpha cells to stimulate the conversion of these molecules to glucose.
Other Functions of Beta Islet Cells
While Beta cells are primarily involved in the production of insulin to regulate blood sugar levels, they are also involved in the production of a number of other essential molecules.
These include:
C-peptide
As the name suggests, C-peptide is a peptide (a short chain of amino acids). It consists of 31 amino acids and is the product of insulin production. For C-peptide to be formed, proinsulin, which is still inactive, is cut at two points through proteolytic action (to release the C-peptide).
The two other parts (which contain internal disulfide bonds) come together to form an active insulin hormone. Although C-peptide has been shown to have a longer life span than insulin (3 to 4 times longer), it's produced in equal amounts (equimolar amounts with insulin).
Because the peptide is produced at the same time and in equal amounts as insulin, it's commonly used to determine the viability of Beta cells and the level of blood sugar. Moreover, it's often used to test the presence of sugar/glucose in urine.
* Because it can inform health care providers about the level of sugar in blood, C-peptide tests are also used to examine or differentiate between type 1 (characterized by little to no insulin/C-peptide) and type 2 diabetes (where the body uses insulin poorly).
Amylin
Also known as islet amyloid polypeptide (IAPP), amylin is a peptide hormone (consists of 37 amino acids) produced by Beta cells. Like insulin, amylin is secreted in response to increased levels of blood sugar. Though it's co-secreted within insulin, studies have shown this hormone to be in lower quantities (insulin: amylin ratio - 100:1).
Given that it's released from the Beta cells, it's normally absent in people with type 1 diabetes (Beta cells are destroyed or not functional). However, for people with properly functioning beta cells, the production of amylin blocks the release of glucagon which in turn decreases the level of blood sugar/glucose. By inhibiting glucagon, glycogen is not converted to glucose.
For this reason, blood sugar level does not increase. Based on a number of studies, amylin has also been shown to reduce the motility of the gastrointestinal tract. For this reason, the hormone is often administered peripherally to help manage body weight by inhibiting food intake.
In a study where a high dose of amylin was administered to mice and rats, researchers noticed that they only ate a small portion of food compared to cases where the hormone was not injected.
GABA
GABA (γ aminobutyric acid) is a neurotransmitter that is also produced by Beta islet cells. The production and release of this molecule by Beta cells is influenced by extracellular glutamine. Once it's secreted, the amino acid binds to GABA Areceptors of the alpha cells and consequently suppresses the secretion of glucagon.
* GABA A receptors are ionotropic receptors. Once the amino acid GABA binds to these receptors, it causes the associated chlorine channels to open allowing chlorine ions (negatively charged chlorine ions) to enter the cell.
With the negatively charged chloride ions entering the cell, they polarize the action potential of the membrane which prevents the cell from firing an action potential. For this reason, the Alpha cells are prevented from releasing glucagon that would otherwise increase blood sugar levels.
* Beta cells have also been shown to express GABA A receptors. As a result, an autocrine GABA signaling system is formed where the cells can influence their own actions by releasing the amino acid.
* Beta islet cells also have a high concentration of zinc. Normally, zinc is taken up through a zinc transporter known as transporter 8. In Beta cells, zinc has been shown to play an important role in the production, storage, and release of insulin.
Alterations to the genes associated with the zinc transporter can cause type 2 diabetes.
Return from Islets of Langerhans to MicroscopeMaster home
References
Denis G. Baskin. (2015). A Historical Perspective on the Identification of Cell Types in Pancreatic Islets of Langerhans by Staining and Histochemical Techniques.
Erez Geron, Sigalit Boura-Halfon, Eyal D.Schejter, and Ben-ZionShilo. (2015). The Edges of Pancreatic Islet β Cells Constitute Adhesive and Signaling Microdomains.
Piero Marchetti et al. (2017). Pancreatic Beta Cell Identity in Humans and the Role of Type 2 Diabetes.
Soltani Nepton. (2012). Beta-Cell Function and Failure.
Links
https://courses.lumenlearning.com/boundless-ap/chapter/the-pancreas/
Find out how to advertise on MicroscopeMaster!