How does an Autoclave Work?
Clean and Sterilize with/without Autoclave
How does an Autoclave work?
Also known as a steam sterilizer, an autoclave is an insulated pressure chamber in which high-pressure steam is used to sterilize (decontaminate) laboratory/clinical material or items.
For different types of material, sterilization time and temperature may vary depending on recommendations. This ensures that given materials are effectively sterilized for use.
In order to understand how an autoclave works, it's important to know the different parts of this device and their respective functions.
Generally, the size and type of autoclave largely depend on the intended purpose. For instance, whereas smaller, tabletop autoclaves are often used in smaller laboratories, private medical facilities or dental offices, larger ones (which tend to be horizontal) are frequently used in hospital laboratories and pharmaceutical offices where they can accommodate larger or more equipment.
Regardless of the type/size of the autoclave, a metal chamber is used in all autoclaves given that it can withstand high steam pressure generated during use. In the past, nickel-clad was used to manufacture the device. However, carbon steel or stainless steel, which is less corrosive, is commonly used today.
The majority of autoclaves, if not all, are also cylindrical in shape. This is particularly important as compared to other shapes (e.g. a cube), a cylinder can easily withstand high pressure. While the exterior of an autoclave may be cuboid for some autoclaves, the inside chamber is generally cylindrical.
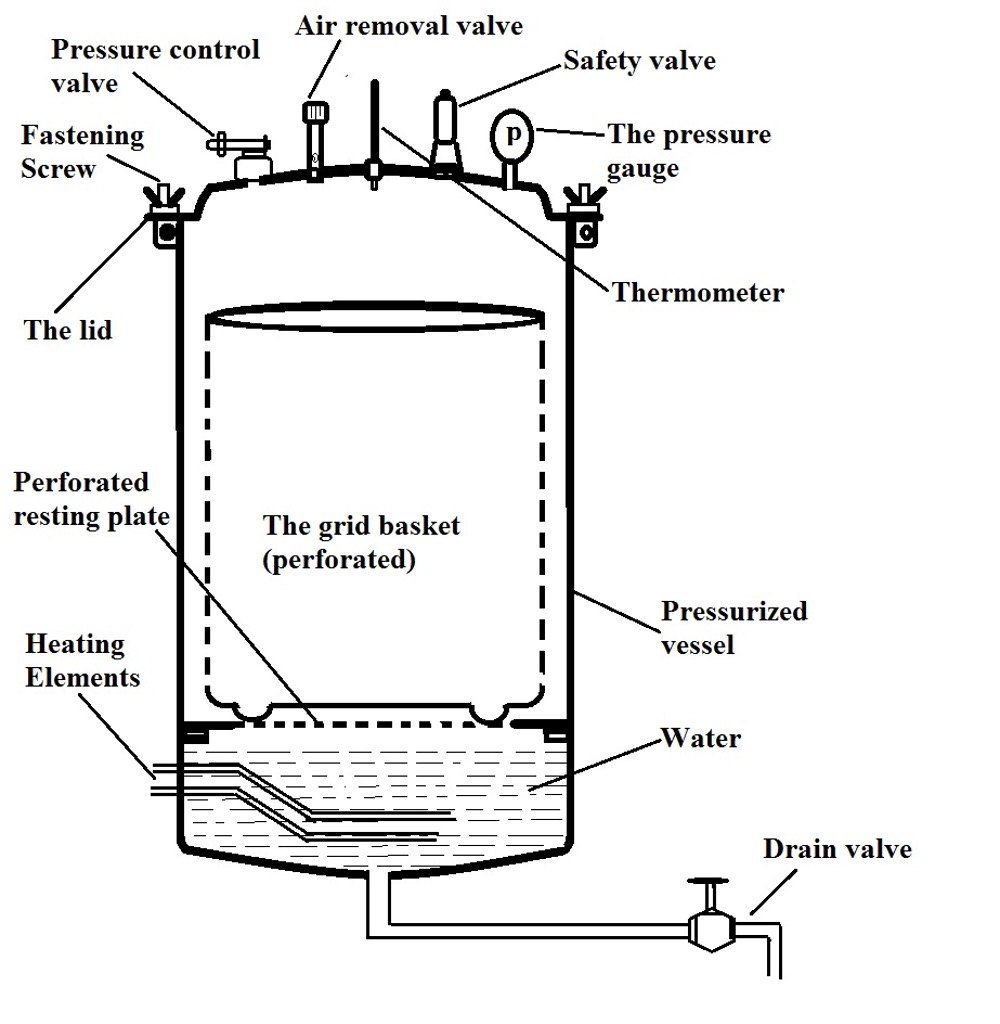
In general, the majority of autoclaves consist of the following parts:
Pressure chamber - This is the primary component of a steam autoclave and generally consists of an inner chamber, where materials being sterilized are placed, which is surrounded by the outer jacket (also known as the outer shell). Within the autoclave body, materials (e.g. equipment or agar solutions etc) are normally placed in the grid basket which is perforated to allow in steam.
These baskets significantly. Some can be easily removed while others are part of the inner chamber (pressure chamber) - As mentioned; the inner chamber is commonly made of stainless steel or carbon steel.
Lid - The lid of an autoclave serves to seal the chamber in a manner that allows for pressure to build up. This is made possible not only by fastening the lid with screw clamps, but also the presence of an asbestos washer which is interpositioned in a manner that prevents steam from escaping. The lid is also very heavy which allows it to withstand pressure as it builds up with increasing temperature.
Some of the main components of the lid include:
· Pressure control valve - The pressure control valve opens when the working pressure has been reached thus keeping the pressure safely below a given upper limit. In the event that this valve fails, the safety valve will open to release pressure out of the chamber.
· Air-removal valve - The air removal valve is used to release steam out of the chamber after the sterilization process is complete
· Temperature gauge (thermometer) - Also located on the lid, a thermometer indicates the temperature inside the chamber which allows a technician to note when the sterilization process starts.
The heating element (electrical heater) - The heating element is located below the chamber and consists of an electric heating system that heats the water in order to produce steam. The element has to be covered with water at all times during use in order to prevent it from burning out. Here, it's always important to ensure that the water level is as recommended. Although having very little water can result in the element burning out, too much water can get into the material being sterilized. The goal of sterilization is to have steam (not water) heat up the material.
Water cooler and drain valve - For the majority of modern autoclaves, a cooling system is installed to cool the water before it is drained out through the draining pipes. Once the water is sufficiently cool, the drain valve is opened to release the water through the draining pipes.
As mentioned, there are several types of autoclaves that include:
· Pressure cooker type - With a capacity of between 5 and 25 liters, this is the simplest type of autoclave. It's portable and commonly used in small heath centers
· Vertical autoclave - This type of autoclave has a capacity of between 60 and 100 liter. It is also double-walled with varying number of electrical installation depending on size.
· Common laboratory autoclave/table-top autoclave - This type of autoclave has a capacity of between 20 and 80 liters and is one of the most common autoclaves in laboratories. The majority of modern table-top autoclaves are automated and consist of a vacuum pump. They also contain several trays on which equipment such as surgical blades etc are placed during sterilization.
· Automatic hospital autoclave/Stationary autoclave - These autoclaves are significantly larger with a capacity of up to 800 liters. Because they are large in size, compared to some of the other common autoclaves, these autoclaves are usually located in a special department (e.g. sterile processing department). They may be fully automated or semi-automated and can be used to sterilize a variety of material.
Sterilization
To sterilize material (surgical equipment, pharmaceutical items, agar solutions etc), the material is first placed in the perforated basket (diaphragm) which is placed just above the water level.
Here, it's important to avoid overcrowding the basket. The material has to be loaded in a manner that will allow the steam to circulate and penetrate the material. In a case where these materials are overloaded, steam may not effectively penetrate some parts preventing the material from being sterilized properly.
In the chamber, placing the items/materials in a secondary container is always recommended. However, the container should also be able to allow steam to penetrate. For this reason, wrapping material in aluminium foils etc should be avoided as they prevent steam from penetrating. Using a secondary container is also important in that it prevents the material from coming into contact with the sides of the inner chamber.
In the case of waste material, autoclave bags are recommended. Some of the best autoclave bags are not only puncture-resistant, but also withstand high pressure thus preventing the material from leaking. However, they can be left open or perforated at the top in order to allow steam to penetrate.
* Clean material and waste material should never be sterilized together.
* Never attempt to open the lip while the autoclave is sterilizing the materials/items.
* Avoid using plastic containers because they can melt.
Once the material/items have been properly placed inside the pressure chamber, making sure that they are just above the water level, the lid is closed and tightly secured with the screw clamps. The electric heater is then turned on and the safety valve adjusted to the required pressure.
Once the water starts boiling, air (mixed with steam) is allowed to escape through the discharge tap. This is particularly important given that it allows the material being sterilized to be exposed to pure steam and not a mixture of steam and air.
At given pressure, this mixture (or air and steam) can result in low temperature and consequently poor sterilization. On the other hand, the air also prevents effective sterilization by preventing proper penetration of the steam.
Because air is denser than steam, the hot steam forms a layer at the top of the cooler air at the bottom. This prevents the steam from effectively penetrating all parts of the material. For this reason, it's important to release the mixture of air and steam and thus retain pure steam.
* To ensure that all air has been removed, the mixture released through the discharge tap is passed into a pail of water through a connecting tube. If air bubbles continue coming into the pail, then air is still present in the chamber. When these bubbles are no longer detected, then all the air in the chamber has been removed.
* Here, air filtration is also important. It prevents potentially dangerous gases from being released into the environment. In addition to the tiny pollutants in the air, filters are also designed to trap viruses and bacteria.
Once all the air has been allowed to escape, the discharge tap is closed which allows pressure to build up to the desired level. For instance, in most cases, the desired pressure is about 15lbs at 121 degrees C. At this pressure, excess steam is allowed to escape through the safety valve.
As soon as the safety valve opens to release excess steam, accompanied by a popping sound, it's time to start counting the holding period (the specified sterilization period). In most cases, material/items are sterilized for about 15 minutes at 15lbs of pressure.
After the specified holding time, the electrical heater is turned off in order to allow the autoclave time to cool. Here, the pressure gauge indicates whether the pressure inside the chamber is equal to the atmospheric pressure. If this is the case, then the discharge tap can be opened slowly in order to allow air to enter before opening the lid to retrieve the sterilized material.
Working Principle
Essentially, sterilization refers to the process through which microorganisms (bacteria, viruses, etc) on the surface of a given substance or material etc are destroyed thus making the substance sterile. Here, the agent used to sterilize is known as the sterilant.
Generally, in many homes and even in some laboratories, given material can be placed in boiling water for about 10 minutes as a means of sterilizing them. However, this method has several drawbacks.
Boiling at 100 degrees C is not enough to kill all microorganisms. While some microorganisms will be destroyed by boiling for several minutes (particularly the non-sporing organisms), it does not completely eliminate all the microbes.
One of the other issues with boiling is the fact that material/substances have to be immersed in boiling water for sterilization. For this reason, some of the material/substances (e.g. waste material) cannot be sterilized using this method. As compared to boiling water, steam as a sterilant has several advantages.
One of the biggest advantages of using steam is that unlike boiling water, steam creates high pressure with increasing temperature. As mentioned, water is added to a certain level so that the material in the basket sits just above the water level. Once the water is added, the lid is tightly closed. As the water is heated, it turns to steam (the gaseous form of water) which occupies more space as compared to water.
As the temperature increases, pressure builds up in the inner chamber. The increasing temperature causes the molecules to vibrate faster. This not only causes the gaseous molecules to take up more space but results in increased pressure.
* Compared to steam molecules, water molecules are tightly packed together which allows water to occupy less space compared to steam.
In the inner chamber, very high pressure is exerted on the microorganisms on the surface of material/substances being sterilized. This is why it's important to ensure that the material are not overcrowded in the inner chamber. Overcrowding prevents steam from penetrating certain areas. Apart from the high pressure created in the chamber, the heat within the chamber also kills the microorganisms present.
When the hot steam comes into contact with the surfaces of the material being sterilized, the steam condenses into a small volume of water. Given that these surfaces are cooler than the steam, latent heat from steam molecules is released to the cooler surface as they condense to water.
As a result, the condensed water molecules become cooler which in turn results in suction of more hot steam to the site. This continues until the site becomes as hot as the steam. In the process, microorganisms located on the surface of the materials/substances are destroyed.
* In order to ensure that all the microorganisms present on the material being sterilized are killed, it's important to sterilize them for a given period of time. generally, this takes about 15 minutes.
How to Clean an Autoclave
Although an autoclave is very effective when it comes to sterilizing various materials and substances, various organic or non-organic substances can accumulate over time. As a result, they can cause damage to the device or cause it to be less effective.
Some of the issues associated with poor autoclave maintenance include staining, chamber corrosion, and even electric hazards, etc. How an autoclave is cleaned is largely dependent on how often it's used. While some autoclaves are only used once every few weeks, others are used daily. For autoclaves that are used everyday, the daily cleaning routine varies from the weekly and monthly cleaning routines.
Daily cleaning - An autoclave that is used daily is more likely to collect more organic and non-organic substances. For this reason, it has to be inspected daily for debris and cleaned. Generally, cleaning the autoclave after each cycle is recommended. Here, however, it's important to ensure that the unit has cooled (make sure that the electric power cord has been disconnected from the power socket) before cleaning to avoid accidental burns.
Generally, cleaning involves wiping with a soft and dry cloth. If stains are present, then a moist cloth with a little detergent may be used. It's always important to inspect different parts of the autoclave in order to ensure that it's thoroughly cleaned. In some institutions, particularly larger laboratories, cleaning involves the use of an ultrasonic cleaner (e.g. Durasonic).
* Accumulation of debris has been shown to prevent the unit from effectively sensing temperature.
Weekly - Here, cleaning should start with using a dry cloth to wipe out debris in the unit.
Once the debris has been removed, the following steps should be taken to thoroughly clean the unit:
· Drain the reservoir - One of the most important steps of the weekly cleaning routine involves draining the reservoir. Here, the process involves filling the tube with distilled water as well as a small amount (about an ounce) of speed clean sterilizer.
Draining is particularly important given that it prevents items from being contaminated with residue that may be present in the fluids. The autoclave is then turned on to run a 30-minute cycle at 121 degrees C before draining the reservoir for a second time.
Once the reservoir has been drained, clean distilled water is added before running a 3-minute cycle at 132 degrees C. Lastly, the reservoir is drained again and the unit allowed to cool.
· Remove the tray plates and wipe any remaining debris and again wipe the inside of the autoclave - A soft and dry cloth is recommended for cleaning in order to avoid damaging sensitive parts of the autoclave including the heater elements and the temperature and level sensor components.
· Once the inside part of the autoclave is clean, carefully re-install the tray rack and plates and ensure that they are properly inserted into the unit.
· Add clean distilled water into the reservoir to the appropriate level (usually marked).
Monthly - Generally, monthly cleaning involves the following steps:
· Run the flush system - This involves draining the reservoir, re-filling with clean, distilled water as well as an ounce of speed-clean sterilizer. This part of cleaning also involves some of the steps mentioned in weekly cleaning (e.g. running 30-minute cycle, draining and re-filling the reservoir again, etc)
· Using speed-clean sterilizer cleaner and a small bristle brush, clean the door gasket, gasket ring and the dam gasket - These parts should be removed in order to be cleaned properly.
· Remove the trays and rack and wipe with a soft dry cloth. The filter should be cleaned using speed-cleaner sterilizer and clean water.
· Testing the biological indicators - This step is normally carried out in order to verify sterility. Normally, this involves sending a processed part to a third party lab for culture.
· Pressure relief valve check - One aspect of monthly cleaning involves pressure relief valve check. This is largely dependent on the type of autoclave, instructions are provided in the operation manual for different types of autoclaves.
Sterilizing without an Autoclave
Without an autoclave, there are several methods that can be used to sterilize various materials/substances.
These include:
Dry-heat sterilization - Given that an autoclave is not used in dry-heat sterilization, a higher temperature is normally used. In addition, the material is exposed to higher temperatures for a longer period of time. For this reason, dry-heat sterilization is generally recommended for material that can withstand high temperatures (particularly non-aqueous materials).
The two main types of dry-heat sterilizers which include; static air sterilizer (using an oven where hot air rises from the bottom of the unit) and forced-air sterilizers (this is where a motor-driven blower allows for heated air to be circulated throughout the chamber).
One of the biggest advantages of dry-heat sterilization is that it can be easily installed and is easy to use. Given that chemicals are not used, corrosion is not a big issue. However, because a very high temperature is used (dry heat), this technique can only be used to sterilize certain materials. The method is time-consuming which is one of the main disadvantages.
Filtration - This method is not FDA-approved and therefore not commonly used for sterilization. However, it's used in some settings and involves the use of membranes with pores that are smaller in size than bacteria. It's usually used to sterilize thermolabile material. Although it's still used in some settings, a good number of scientists have questioned its effectiveness.
Ionizing radiation - This method of sterilization involves the use of cobalt 60 gamma rays or electron beams. Although it has been used to sterilize a number of materials/substances including medical devices and tissue, ionizing radiation, like filtration, is not yet FDA-cleared.
It's one of the more dangerous methods and therefore only used by a few well-trained technicians. In addition to being a costly sterilization method, this method has also been shown to affect the integrity of cells in tissues (causing mutations in DNA).
Gas sterilization - Gas sterilization involves the use of various highly volatile substances. Because of their nature, they have to be mixed with other gases (inert gases) in order to reduce their toxicity. The efficiency of gases used here (e.g. ethylene oxide) is largely dependent on the concentration of the gas.
Some of the other methods used for sterilization include:
· Using infrared radiation - Infrared radiation is commonly used to sterilize certain medical equipment
· Peracetic acid (vapor) - Although this method has not been cleared by the FDA, it has been used to destroy various microorganisms within a short period of time
· Formaldehyde steam - In this method, the material being sterilized is exposed to a series of formaldehyde steam in a chamber
Of Interest in the Laboratory:
|
Digital Microscope Camera and Digital Microscope Camera Adapter Microscope Slides and Cover Slips |
Return to Laboratory Centrifuge
Return to Laboratory Accessories
Return from Autoclave information to MicroscopeMaster home
References
Boston Career Institute (BCI Inc.). (2014). steam sterilization, how it all works.
Festus Oyawale and A. E. Olaoye. (2007). Design and Construction of an Autoclave.
Louise Simmers. (2001). Diversified Health Occupations.
Mana Sezdi and Gamze Yoleri. (2014). Sterilization performance of autoclave units on cannular materials.
M Dion. (2013). Steam Sterilization Principles.
Links
https://www.cdc.gov/infectioncontrol/guidelines/disinfection/sterilization/other-methods.html
https://www.thomasnet.com/articles/process-equipment/all-about-autoclave-bags/
Find out how to advertise on MicroscopeMaster!