How and Where are Memory Cells Produced?
What are Memory Cells?
In the immune system, the term memory cells is used to refer to a group of cells with the capacity to "remember" or recognize a stimulus (antigen, pathogen) from a previous encounter and effectively mount a response.
Given that the cells have "memory" of the stimulus, even a smaller stimulus is rapidly identified allowing for a quicker and effective secondary immune response. As they are retained for a long period of time after the initial encounter, memory cells are especially important in that they can respond rapidly and more strongly in the event of future incursions to fight off the infection.
Memory cells of the immune system include:
- Memory B cells
- Memory T cells
- Memory or memory-like natural killer cells
How and Where are Memory Cells Produced?
The production of memory T cells start with the activation of T cells (T lymphocytes). Following the production of T cells in the bone marrow, they migrate to the thymus where they mature further. Here in the thymus, one of the most important events involves the expression of T cell receptors following recombination of genomic DNA sequences as the T cells mature.
This is especially important given that T cell receptors play an important role in the activation of these cells. These receptors are also unique and thus result in T cell specificity. This maturation process results in the production of naive T cells which are incapable of mounting a response against an invading pathogen.
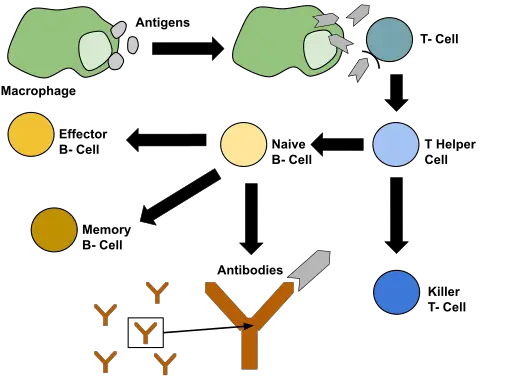
A naive T cell is activated when it interacts with an antigenic peptide. Here, such peptides are presented by specialized cells known as antigen-presenting cells (e.g. dendritic cells). Having ingested the pathogen, these cells (antigenic presenting cells) bear the antigenic peptides of the pathogen on the major histocompatibility complex (MHC class I or class II) - MHC are molecules that are expressed on the surface of antigen-presenting cells where they bind antigenic molecules.
Following interaction between the naive T cells and the antigen-presenting cells, their receptors are able to recognize the antigen bound to the major histocompatibility factor which ultimately results in their activation. However, this process involves a number of other events before T cells are finally activated.
For instance, during the identification of the antigen, the T cell receptor has been shown to associate with a co-receptor (CD4 or CD8 depending on the T cell) and consequently bind to the major histocompatibility complex to enhance the interaction between the antigen-presenting cell and T cell.
* While the presence of given antigenic molecules play an important role in T cell activation, studies have shown that a number of other signaling molecules are essential for complete activation. Here, some of the molecules associated with this activation include CD28 and some cytokines etc.
Activation of T cells does not directly result in the production of memory T cells. Rather, it results in the differentiation of the T cells to produce two categories of T cells that include helper T cells and cytotoxic T cells. These are functional/active cells and thus involved in various responses.
For instance, while cytotoxic T cells are involved in the destruction of cancer cells as well as infected cells, helper T cells, as the name suggests, are involved in the activation of B cells and cytotoxic T cells. As such, they promote some of the other immune cells to effectively carry out their functions.
Following the elimination of the invading pathogen by the effector cells (e.g. cytotoxic cells) during the primary response, where the T cells first encounter the invading pathogen, there is a significant decline of T cell population.
* Effector T cells can migrate to inflamed tissue where they destroy infected cells and associated pathogens in these cells.
* The population of expanded effector T cells is reduced through apoptosis following the elimination of the pathogen.
Although many of the T cells die off once the pathogen is eliminated, a small population of T cells is retained in various tissues (e.g. lungs, skin, and gut) as well as the secondary lymphoid organs. These cells have a memory of the pathogen, or antigens associated with the pathogens, and are therefore known as memory T cells.
Compared to naive T cells, memory T cells only require a little activation to respond. Moreover, they have been shown to have a higher proliferative potential which allows for a rapid and stronger effector response.
On the other hand, memory T cells can easily traffic/migrate through the peripheral tissue and secondary lymphoid organs (SLO) which allows for better access to various tissues.
* Memory T cells are also long-lived which allows them to protect against future infections against specific invaders. This is especially true for memory T cells found in peripheral tissues given that they have been shown to be more resistant to apoptosis (natural cell death) compared to those found in circulation.
Types of Memory T Cells
There are two main types of memory T cells which include central memory T cells and effector memory T cells. Central memory T cells (Tcm) are characterized by high levels of adhesion markers, low levels C chemokine receptor type 7 (CCR7), as well as low levels of KLRG-1.
Effector memory T cells, on the other hand, are characterized by low CD62L levels, high levels of KLRG-1, as well as low levels of CD127. Unlike central memory T cells, effector memory T cells have been shown to have a reduced proliferative potential.
Central memory T cells are commonly found in various secondary lymphoid organs (tonsils and lymph nodes) and can secrete such cytokines as CD40L ligand, IFNγ, and Interleukin 2. Effector memory T cells, on the other hand, are commonly found in non-lymphoid peripheral tissues like the liver and lungs.
However, they can also migrate to and from circulation. Some of the cytokines secreted by these cells include Interleukin 4 and IFNγ.
* Both central and effector memory T cells are involved in secondary immune responses.
Some of the other types of memory T cells include:
Tissue-resident memory T cells (Trm) - Unlike the other memory T cells, these memory cells reside in tissues and do not enter circulation. Because they are located in such locations as the digestive tract, skin, and the female reproductive system, etc., they act as the first line of defense in these regions.
Here, their response has also been shown to be more rapid and effective compared to the other memory T cells given that they do not have to migrate but rather act locally. Some of the characteristics associated with tissue-resident memory T cells include surface markers like CD103 and CD69, low L-selectin levels, as well as a high expression of CD44.
Memory regulatory T cells (mTreg) - As the name suggests, these cells play an important role in the maintenance of immune homeostasis, modulating inflammation responses, as well as inhibiting autoimmune reactions.
Stem cell-like memory T cells - Unlike most memory T cells, those with stem-like properties (Tscm) have been shown to share some similarities with naive T cells. They are characterized by a number of molecules on their surface including CCR7, CD27, and CD62L, among others.
* In the absence of antigens, interleukin 7 plays an important role in maintaining memory T cells.
Memory B Cells
Like memory T cells, B cells also retain the memory of given antigen which allows them to respond rapidly.
The production of memory B cells may involve several routes that include:
T cell-dependent Memory B cell formation
T cell (T helper cells) responses have been shown to play an important role in the production of memory B cells. Once they are activated (by the presence of antigens), follicular dendritic cells, Helper T cells (follicular T helper cells), and B cells come together. B cells and T cells interact through the CD40 ligand on their surfaces to form a germinal center within the center of B cell follicles in secondary lymphoid organs.
Here, T cells have been shown to produce cytokines that maintain the germinal center while follicular dendritic cells serve to retain intact antigens within specialized complexes. Activated by antigens, some of the B cells proliferate and undergo differentiation to produce plasma cells capable of producing antibodies against foreign antigens.
While antigen stimulation and support from follicle T helper cells promote survival of the B cells, some of these B cells are unable to compete and die. In a region of the germinal center, B cells compete with each other for antigen resulting in high affinity to the antigen form some of the B cells. The B cells with high and specific affinity for antigen become memory B cells, also known as antibody-producing plasma cells.
* When different types of pathogens invade the body they influence the development of new germinal centers in the secondary lymphoid tissue. This is important in that it ensures the diversity of antigen-specific B cells that can respond to specific antigens.
T cells independent memory cells
In human beings, T celli independent activation of B cells generally involves the cross-linking of B cell receptors by non-protein antigen epitopes. This results in the production of plasma cells that secrete IgM. Unlike the T cell receptor-dependent B cell activation, this type of activation does not produce memory B cells. In mice, however, studies have shown this mechanism to produce memory-like cells.
* Apart from their ability to survive for an extended period of time, these cells are generally characterized by IgM. However, it's not well understood whether they are capable of continued proliferation once they are produced.
Natural killer memory cells (also referred to as memory-like natural killer cells)
While natural Killer cells (NK) were initially through to be short-lived innate cells, studies have shown that like memory T and B cells, these cells can develop antigen-specific memory for a few pathogens.
Like memory T cells, natural killer cells also go through several stages before memory cells are produced. Here, the first two stages include activation and expansion of natural killer cells. During the activation phase, studies have shown viral infections such as the Acute MCMV infection in mice to influence the production of cytokines like IL-18and type I interferon.
Some of the other proteins that may be released here include IFN-y, interleukin 12, and transcription factor STAT4. As some of these cytokines activate natural killer cells, some, like IL12 and IL18, also promote the expression of the transcription factor Zbtb32 which protects and directs the proliferation of the natural killer cells.
Once they are activated, natural killer cells can target and destroy infected cells (infected with viruses). Here, proliferation allows them to increase in number in order to effectively carry out this function.
The third phase is known as the contraction and survival stage and occurs when the infection has been cleared. This is also the stage at which memory cells are produced.
Following viral clearance, the pro-survival molecule Bcl-2 is down-regulated resulting in the reduction of the number of natural killer cells (contraction). This, however, is a controlled process that allows some of the cells to survive.
One of the survival mechanisms by some of the natural killer cells involves the removal of damaged mitochondria through a process known as autophagy. This allows a small population of cells to survive the contraction phase. These cells then go on to form memory natural killer cells.
Some of the characteristics associated with these cells include a high expression of several molecules including CD43, Ly6C, and KLRG1. As well, they express lower levels of CD27 which has led researchers to compare them (phenotypically) to memory T cells.
Being highly sensitive to different types of viral infections (with high specificity), natural killer memory cells can respond rapidly to clear the infection within a short period of time compared to a primary response. Compared to activated natural killer cells, these cells also have a longer life-span and can be found in a number of locations including the liver and spleen.
Return from How and Where are Memory Cells produced? to MicroscopeMaster home
References
David L. Woodland & Jacob E. Kohlmeier. (2009). Migration, maintenance and recall of memory T cells in peripheral tissues.
Kyla D. Omilusik & Ananda W. Goldrath. (2017). The origins of memory T cells.
Nathan D. Pennock et al. (2013). T cell responses: naïve to memory and everything in between.
Michael D. Rosenblum, Sing Sing Way, and Abul K. Abbas. (2015). Regulatory T cell memory.
Timothy E. O’Sullivan, Joseph C. Sun, and Lewis L. Lanier. (2015). Natural Killer Cell Memory.
Links
Find out how to advertise on MicroscopeMaster!
![Processes involved in the primary immune response by Sciencia58, Domdomegg, [1], Fæ, Petr94, Manu5, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons Processes involved in the primary immune response by Sciencia58, Domdomegg, [1], Fæ, Petr94, Manu5, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons](https://www.microscopemaster.com/images/512px-Primary_immune_response_1.png)