Antigen Vs Antibody
In Blood, Hepatitis B, Hepatitis C and Malaria
Overview
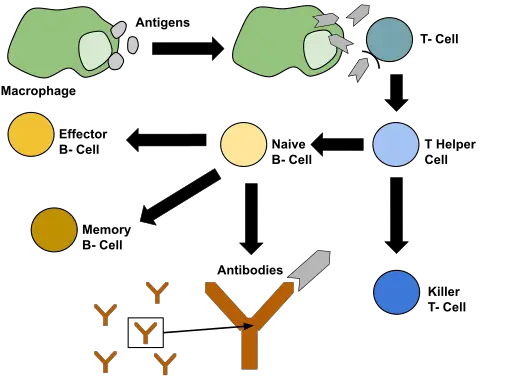
Essentially, an antigen refers to a substance (they are generally protein or polysaccharide molecule) with the capacity to elicit an immune response. In particular, they can trigger the production of antibodies and bind to these antibodies.
These substances may originate from the external environment (outside the body) or formed in the body.
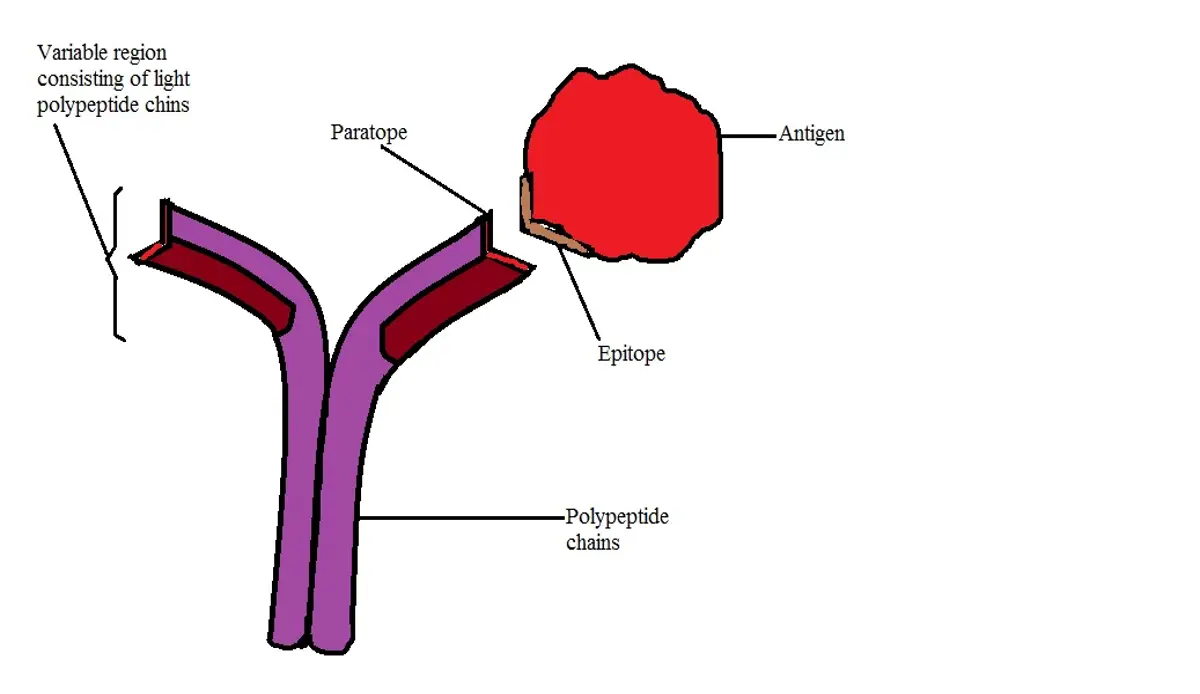
Some of these molecules/substances (known as self-antigens) are tolerated because they are not identified as foreigners or invaders. An antibody, on the other hand, is an immunoglobulin that is produced in response to the presence of an antigen. They consist of polypeptide chains and are capable of combining with given antigens.
Also known as immunoglobulin (Ig), antibodies are Y-shaped and contain molecules known as paratopes on their tips. This is the part of the antibody that recognizes and binds to the antigen (at the epitope of the antigen). Paratopes are specific to epitopes which allows for a specific response to a given antigen.
Blood - Antigen Vs Antibody
Red Blood Cells
Antigens (which consist of sugars or proteins) can be found on the surface of red blood cells and serve as a basis for blood grouping. As is the case with various other cellular components, the DNA is involved in the production of these molecules.
In particular, the DNA is involved in the production of given types of enzymes that catalyze the transfer of sugar units that form the antigens ABO.
Apart from these molecules (sugar units), the DNA is also involved in the production of another group known as the Rhesus (Rh) factor. Unlike ABO, the RH blood group consists of proteins. Here, a gene known as RhD is responsible for encoding the D antigen which is then located on the surface of red cells (on the cell membrane).
If this large molecule (D) is present, then an individual is said to be rhesus positive (RhD positive). However, in the event that it's absent, then an individual is rhesus negative.
* While some people may have the gene responsible for encoding the D antigen, this does not necessarily mean that they are capable of producing the antigen.
* While only ABO and Rh blood groups systems are of clinical significance, studies have shown there to be 36 blood group systems.
In human beings, as is the case with other animals, it's the antigens that are expressed on the surface of their red cells that determine the blood group of an individual. With regards to the ABO system of blood grouping, there are four main blood types that include A (group A have the A antigen on their red cells), B (group B have B antigen on their red cells), AB (Group AB have AB antigens on their red cells), O (lack the A and B antigens).
* Group O was initially known as blood group C.
Given that an individual’s blood type is determined by the type of antigens on their red cells, there are antibodies to the antigens present. However, these antibodies are not located on the surface of red cells. For an individual with blood type A, then they have anti-B antibodies in their serum/plasma.
An individual with blood type B on the other hand will have anti-B antibodies in their serum while an individual with blood type O has both anti-A and anti-B antibodies in their plasma.
Because a person with blood type AB has both antigens, they do not have antibodies. For this reason, they can receive blood from any of the other groups given that they do not have antibodies that will target the new blood cells.
* Given that Rh D is also an antigen, the presence of this antigen can trigger the production of antibodies. A good example of this is the production of Rhesus antibodies that are produced by Rhesus negative mothers in response to a Rhesus positive fetus.
* The ABO antigens are expressed by the H and ABO genes.
Antigens of red blood cells are also referred to as isoantigens/agglutinogens while the corresponding antibodies are also known as isoantibodies/agglutinins.
Agglutination Reaction
Blood agglutination occurs when antigens on the surface of red cells are identified as being foreign. For instance, as already mentioned, individuals with blood type A produce antibodies against antigens that an individual does not have (Anti-B).
In a scenario where an individual with blood type A receives a blood transfusion from an individual with blood type B (or AB), then the new red cells will be targeted because their antigens are identified as being foreign. This is known as an ABO incompatibility reaction.
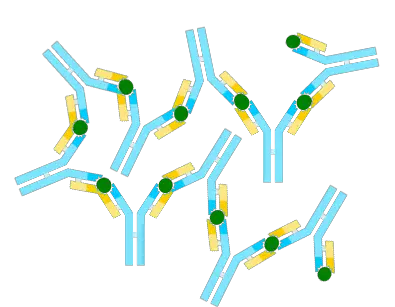
Here, the presence of the foreign antigen triggers the production of antibodies by B lymphocytes which attach to the antigens causing them to adhere. Because the antibodies produced have Y-shaped arms, they are able to attach to several foreign antigens (and thus to the foreign red cells) causing them to clump.
* Clumping of red cells is dangerous given that it can cause blockage of small vessels thereby limiting the transportation of oxygen and nutrients required by body tissues.
Leukocytes and Platelets
Apart from the antigens found on the surface of red blood cells, studies have also shown white cells and platelets to have antigens. The antigens found in leukocytes are known as HLA (Human leukocyte antigens) antigens while those that are found in platelets are known as HPA (Human platelet antigens) antigens.
Both these antigens originate from the single nucleotide polymorphisms in genes that are responsible for encoding the glycoprotein that are expressed on the surface of platelets. Therefore, while they are anucleated, platelets have been shown to the primary source of the antigens (HLA class I) found on blood leukocytes.
* The antigens expressed on the surface of leukocytes are also involved in tissue rejection.
Hepatitis B
Hepatitis B is a viral infection that affects the liver (causing acute and chronic liver disease). It's caused by the hepatitis B virus (HBV) and can be transmitted from one individual to another through body fluids, blood, or through sexual contact.
* Hepatitis B belong to a family of viruses known as Hepadnaviruses.
The virus consists of a double-stranded DNA that is surrounded by a lipoprotein envelope. The surface antigen (HBsAg) molecule is located on this envelope. Based on molecular studies, HBsAg has been shown to be a complex macromolecular structure that consists of protein (p-25), glycoprotein (gp-30), and lipid.
While the major protein and glycoprotein have similar amino acid sequences, their difference lies in the fact that the glycoprotein contains a carbohydrate. They are also divided into four main groups based on group-specific determinant.
While all the HBsAg have been shown to contain the group-specific "a" determinant, some may either contain "d" or "y" determinant in addition to the "a" determinant. Some also may contain "w" or "r" determinant in addition to the "a" determinant. Therefore, they are divided into four main groups that include; ayw, adw, adr, as well as ayr.
In the body, Anti-HBs antibodies (HBsAb) are produced by B cells and plasma cells following an infection. However, these antibodies are also produced following vaccination against the virus.
Following a vaccination or an initial infection, this antibody (Hepatitis B Surface Antibody) can protect an individual from the virus in the future and thus prevent it from being spread to other people.
Apart from HBsAb, individuals also produce a Hepatitis B Core Antibody (HBcAb) in response to acute hepatitis B. However, this particular antibody does not provide protection against the virus. Regardless, its detection is important in that it is indicative of exposure to hepatitis B.
* The HBsAg-anti-HBs Complex induces humoral and cytotoxic T-cells to action.
* In cases where the infection occurred a long time ago, Anti-HBs tend to decrease in number over time and ultimately become undetectable.
Test
A hepatitis B blood test tests for the presence of HBsAg (Hepatitis B surface antigen), HBsAb (Hepatitis B surface antibody) as well as HBcAb (Hepatitis B core antibody). In the event that an individual tests positive for the antigen, this is indicative of a hepatitis B infection. However, additional testing is required to determine whether the infection is acute or chronic.
A positive test for Hepatitis B surface antibody indicates that an individual is protected against the virus. In most cases, the immune system fights the infection and results in full recovery. However, protection may also result from a hepatitis B vaccination.
On the other hand, if an individual tests positive for Hepatitis B core antibody, then this is indicative of a current or past infection. Given that this antibody does not provide protection against the virus, it's important that the two other tests mentioned above are carried out.
Hepatitis C
Hepatitis C is a liver infection caused by the hepatitis C virus. This infection can be fatal, leading to excessive liver damage. The virus is very small in size, ranging from 55 to 64nm and consists of a positive-sense single-stranded RNA and an envelope.
Being a blood-borne virus, the hepatitis C virus is commonly transmitted through sharing needles. However, it can also be transmitted through blood transfusion if proper measures are not taken beforehand.
The HCV core antigen (HCV cAg) is a component of the nucleocapsid structure and serves as a marker of infection. In response to an infection, the body produces Anti-HCV antibodies (Hep C antibody). Made by leukocytes, this antibody specifically targets the hepatitis C virus and binds to it which in turn triggers an immune response.
* Broadly neutralizing antibody (bNAb) produced in response to hepatitis C infection play an important role in targeting the viral envelope thus blocking the infection.
Test
There are three main types of tests for Hepatitis C.
They include:
· HCV antibody test - This test is aimed at determining the presence of antibodies produced in response to the infection. The presence of these antibodies is indicative of a current or past infection.
· HVC RNA test - Unlike tests that investigate the presence of antibodies or antigens, this test is used to investigate the presence of viral RNA (of Hepatitis C) in blood.
· HCV genotype test - This particular test investigates the strain or subtype of hepatitis C.
Malaria
Malaria parasites (Plasmodia) are single-celled protozoa that belong to the phylum Apicomplexa. Currently, over 200 species of the genus Plasmodium have been identified. The majority of these species are parasites of various hosts including mammals and birds etc.
While there are many Plasmodium species, only a few are responsible for human disease. These include Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae, Plasmodium knowlesi, and Plasmodium ovale.
In the infected host, such malaria parasites as Plasmodium falciparum have been shown to express a number of antigens known as variant surface antigens. These antigens are encoded by the var genes located in the genome of the parasite.
Unlike some of the other antigens that are commonly expressed on the surface of the organism (extracellular bacteria etc), these antigens (variant surface antigens) are normally expressed on the infected cell (erythrocytes). As a result, the cell becomes the target of destruction.
* Apart from the antigen proteins expressed on the surface of infected cells, researchers also discovered that a protein antigen of the plasmodium is expressed on the surface of the gamete and sporozoite forms of the parasite.
In human beings, the antibodies are produced one or two weeks after the initial infections. These antibodies may be produced following infection by any of the 5 Plasmodium species mentioned above. Here, specific antibodies are produced for given parasites and may persist in the body for several months (or years) after the infection has been cleared.
One of the most common antimalarial antibodies is the IgG (Immunoglobulin G) antibody. While this antibody is commonly produced in adults, particularly in endemic areas (e.g. parts of sub-Saharan Africa), studies have shown that it's capable of being transferred to the fetus from the mothers blood thus providing protection against malaria parasites in their first year of life.
The antigens exposed on the surface of infected cells are accessible targets on which the antimalarial antibodies bind (during Opsonization). The complex stimulates the production of phagocytic cells that are responsible for phagocytosis of the infected cell.
Given that malaria parasites invade erythrocytes, phagocytosis of infected cells is particularly important as both the damaged cells and the parasites are destroyed in the process.
Return from Antigen Vs Antibody to MicroscopeMaster home
References
Antoine-Marie Diatta et al. (2004). Relationship of Binding of Immunoglobulin G to Plasmodium falciparum-Infected Erythrocytes with Parasite Endemicity and Antibody Responses to Conserved Antigen in Immune Individuals.
CHEMICON International, Inc. (1998). Introduction to Antibodies.
Laura Dean. (2005). Blood Groups and Red Cell Antigens.
Stanca M. Ciupe, Ruy M. Ribeiro, and Alan S. Perelson. (2014). Antibody Responses during Hepatitis B Viral Infection.
Valeria de Freitas Dutra et al. (2019). Allele and haplotype frequencies of human platelet and leukocyte antigens in platelet donors.
Links
https://courses.lumenlearning.com/boundless-microbiology/chapter/antibodies/
Find out how to advertise on MicroscopeMaster!