Leukocytes
Definition, Function, Count, in Urine and Microscopy
Definition: What are Leukocytes?
Leukocytes are the major cellular components of the inflammatory and immune system. While they only make up about 1 percent of the blood in the body, leukocytes play an important role in protecting the body from infections/diseases caused by various microorganisms (e.g. bacteria, amoeba etc) and other types of parasites (filarial worms etc).
Moreover, they are involved in various allergic reactions and contribute to the repair of damaged tissue as well as the elimination of tumorous cells. In some cases, however, leukocytes may be the cause of diseases as is the case with autoimmune diseases and non-hemolytic transfusion reactions in human beings.
Depending on whether they contain granules or not, there are two major types of leukocytes that can be found in blood, cerebrospinal fluid as well as various body tissues where they remain for several hours or a few days depending on the type of cells.
Cells of the immune system include:
- Monocytes
- Lymphocytes
- Basophils
- Eosinophils
- Neutrophils
Production of Leukocytes
Lymphocytic and Myelocytic Lineage
In the body, white blood cells are formed through two major lineages namely, the lymphocytic lineage and the myelocytic lineage. Whereas the lymphocytic lineage results in the production of lymphoblasts, the myelocytic lineage produces the other types of white cells of the immune system.
Lymphocytic Lineage
In the embryo, lymphocytes (T and B lymphocytes) are produced in the mesenchymal cells (stem cells located in the wall of the yolk sac), liver and spleen. However, in adults, these cells are formed in the stem cells located in the bone marrow (red bone marrow).
Here, it's worth noting that all blood cells arise from the nucleated reticuloendothelial cell known as hematocytoblast in the bone marrow. As such, it is the stem cell that acts as the precursor of the different types of blood elements in the body.
The hematocytoblast then divides into the myeloid and lymphoid stem cells. In the Lymphocytic lineage, the lymphoid stem cell produces the lymphoblast under the influence of IL-3, IL-5 and granulocytic colony-stimulating factors.
The lymphoblast then undergoes proliferation and differentiation to form the prolymphocyte which in turn develop to form the lymphocytes (B and T lymphocytes).
The mature lymphocyte produced by prolymphocyte in the bone marrow (B lymphocytes) is released from the marrow from where it migrates to the bloodstream. This lymphocyte is functional and thus capable of responding to attacks.
The T lymphocyte, however, is not functional and thus has to travel to a lymphatic gland (or primary lymphoid organ) where it matures further.
* From the bone marrow, lymphocytes migrate to the bloodstream through capillaries known as sinusoidal capillaries.
From the bone marrow, the B lymphocytes, which are mature, travel straight to the bloodstream from where they can then reach the secondary lymphoid organs (spleen, lymph, tonsils modes etc) for further maturation.
T lymphocytes, however, have to travel to the primary lymphoid organ (Thymus) where they have to mature (and become functional) before migrating to the bloodstream and ultimately to the secondary lymphoid organs.
Myelocytic Lineage
As is the case with the lymphocytic lineage, the myelocytic lineage also starts with the division of the hematocytoblast to form the myeloid stem cell.
* The myeloid stem cell is also the origin of platelets and red blood cells. Here, red blood cells and platelets are formed under the influence of EPO and TPO respectively.
Under the influence of IL-3, IL-5 and agranulocytic colony-stimulating factors (aG-CSF) myeloid stem cells give rise to the monoblast that is committed to developing into a monocyte. Here, the monoblast first develops into a promonocyte that further develops into monocyte.
While granulocytes are also produced under the influence of IL-3 and IL-5, they require the presence of granulocytic stimulating factor (G-CSF). Under the influence of these three factors, myeloid stem cell give rise to the myeloblast that can further divide into three different lineages; basophil, eosinophilic and the neutrophilic lineages.
Here, the myeloblast gives rise to three different types of cells that may include the basophilic promyelocytes, eosinophil promyelocytes as well as the neutrophilic promyelocytes that in turn give rise to basophilic myelocytes, eosinophilic myelocytes, and neutrophilic myelocytes respectively. These cells, which are partially developed, ultimately produce mature and well-developed basophils, eosinophils and neutrophils.
* Mature and function granulocytes develop from cells referred to as band cells (basophilic band cells, eosinophilic band cells, and neutrophilic band cells) and are characterized by lobed (or s-shaped) nucleus and granules.
* From the bone marrow, basophils, eosinophils, and neutrophils travel to the blood through the sinusoidal capillaries.
Movement
How Leukocytes Migrate to the Site of Action
While leukocytes are carried by the bloodstream to different organs/tissue where they may reside for a few days, they have the ability to migrate by adhering to the endothelium (vascular endothelium).
Adhesion of leukocytes to vascular endothelium is made possible by the presence of oligosaccharide molecules on the surface of these cells (leukocytes) and proteins known as selectins on vascular endothelium.
Through the transitory interactions between these molecules, leukocytes are able to adhere to the endothelium. Blood flow along the endothelium provides the force required to produce rotational motion of the cells known as rolling.
For the most part, this behavior (rolling) is quantified by assessing the number of cells that pass a given point.
This type of movement is part of leukocyte extravasation that involves the following steps:
· Chemoattraction - Activation of specific leukocytes by the presence of pathogens. Here, such cytokines as IL-1 and other chemokines stimulate endothelium cells and leukocytes to prepare for rolling adhesion.
· Rolling adhesion - The process through which leukocytes roll along the inner surface of endothelium having adhered to these walls. Movement is made possible by the formation and breaking of transitory bonds between molecules of endothelial cells and leukocytes.
· Tight adhesion - This is stimulated by chemokines that cause surface integrins to switch from low to high affinity state that ultimately causes immobilization of leukocytes.
· Transmigration - Here, leukocytes spread out across the surface of the endothelial cells and form pseudopodia. This allows them to squeeze through the spaces between endothelial cells (through a process known as diapedesis) and migrate to the affected site.
Characteristics and Functions
Generally, leukocytes are divided into two groups that include granulocytes and agranulocytes. Granulocytes include neutrophils, eosinophils, and basophils that are characterized by lobed nuclei and granules. Agranulocytes, on the other hand, include lymphocytes and monocytes that lack granules found in granulocytes.
In general, leukocytes play an important role in protecting the body from invading microorganisms as well as removing debris and mutated cells. In doing so, they allow various cells of body tissue to continue functioning properly.
While all leukocytes are involved in immune responses in order to defend the body, this is achieved in different ways by the different types of leukocytes.
Granulocytes
Neutrophils
Neutrophils make up the majority of leukocytes (between 50 and 70 percent) and tend to be significantly larger than red blood cells (10 to 12 um in diameter). They contain fine, numerous granules that appear light lilac when stained with neutral strains. They contain a lobed nucleus that may contain 2 to 5 lobes depending on age (of the cells).
As efficient phagocytes, neutrophils are the first line of defense. Using the lysozyme in their granules, they break down bacterial cell walls thus killing them. In addition, they produce proteins known as defensins through which they bind and destroy the plasma membrane of both fungus and bacteria thus destroying them.
Eosinophils
Eosinophils make up between 2 and 4 percent of the total white blood cells. They contain a bi-lobed nucleus (but some may have three lobes) and measure between 10 and 12um in diameter. As granulocytes, they are also characterized by granules that may appear red or orange following staining.
Like neutrophils, eosinophils are capable of phagocytosis. Unlike neutrophils, however, the granules of eosinophils contain antihistamines that serve to counteract the actions of histamines. They have also been shown to contain various toxic molecules that can kill such parasitic worms as filarial worms.
Basophils
Basophils make up between 0.5 and 1 percent of the total white blood cell count and measure between 8 and 10um in diameter with a bi-lobed nucleus. Their granules are larger in size and will appear dark blue in color following staining.
Like mast cells, basophils promote inflammatory responses. This is achieved by the release of histamines that enhances inflammation. They also release heparin that inhibits blood clotting.
Agranulocytes
As compared to granulocytes, agranulocytes contain much smaller granules that are not clearly visible. Unlike the nucleus of granulocytes, the nucleus of agranulocytes are not lobed and thus have a simple shape that may have a small indentation.
Lymphocyte
Lymphocytes are products of the lymphocytic lineage and develop in the lymphatic tissues. They makeup between 20 and 30 percent of the total white blood cell count and vary significantly in size. For instance, whereas smaller lymphocytes range between 6 and 9 um in diameter, larger ones can measure between 14 and 17um in diameter.
There are three types of lymphocytes that include:
B and T cells - B and T cells are involved in specific immunity and thus act against given disease causing microorganisms. Whereas B cells are capable of producing antibodies that bind to given pathogens (humoral immunity), T cells attack and destroy invading microorganisms and abnormal cells.
* Both B and T cells can form memory cells that, after exposure to given pathogens, can recognize such pathogens in the future and thus mount a rapid response against them.
* Memory cells can exist for many years following maturation.
Monocytes
Like lymphocytes, monocytes are also agranulocytes. Unlike lymphocytes, however. monocytes are products of the myelocytic lineage. They make up between 2 and 6 percent of the total white blood cell count and can be recognized by the shape of their nuclei that tends to be horseshoe-shaped.
They are also larger in size when compared to a number of other leukocytes, measuring between 12 and 20um in diameter. When they leave the blood, monocytes are known as macrophages. They destroy invading microorganisms and other debris (worn-out cells etc) through phagocytosis, but also release various chemicals that activate and recruit other leukocytes to the affected site.
Leukocytes in Urine
A urinalysis test (urine test) may reveal leukocytes in urine. Depending on the number of leukocytes, this may be an indication of inflammation/infection along the urinary tract (urinary tract infection- UTI).
For the most part, high amounts of leukocytes in urine has been associated with an infection in the kidney or bladder. However, it may also indicate an infection in the prostate and urethra.
Some of the infections of the urinary tract include:
- Cystitis
- Urethritis
- Prostatitis
* A urine test (urinalysis) involves the use of a dipstick test kit that can detect the presence of leukocyte esterase in urine once it is immersed in a sample of urine.
* The presence of nitrites in a urine sample is, in some cases, indicative of bacterial infections.
Leukocytes/White Blood Cell Count
Because of their functions in the body, the number of leukocytes in the body can vary significantly. This, for the most part, is dependent on whether or not an infection has occurred.
The number also varies based on several other factors such as age and sex. Through a white blood cell count, it's possible to determine whether there is an infection or other undiagnosed conditions such as autoimmune diseases.
* For healthy individuals, the normal white blood cell count ranges between 5,000 and 10,000 cells per microliter of blood for men and 4,500 and 11,000 for women.
To determine the amount of each type of leukocyte in the body, automated or manual differential techniques can be used:
Automated Differential Blood Count
One of the methods used for leukocyte count is fluorescence flow cytometry. Using this technique, it is possible for specialists to assess the physiological and chemical properties of different types of cells.
Basically, the technique involves aspiration and proportioning of a blood sample that is then diluted in order to obtin the pre-set ration. Using a proprietary marker, the sample is then labeled before it is introduced into the flow cell. In the flow cell, the sample is then illuminated by a semiconductor laser beam.
This not only provides information regarding the internal structure of the cells, but also allows for the number of different types of cells to be counted.
* Automated leukocyte count takes less time and tends to be less expensive when compared to the manual technique. This is because it allows for thousands of leukocytes to be examined within a short period of time as compared to manual where only 100 to 200 cells can be examined.
Manual Differential Blood Count
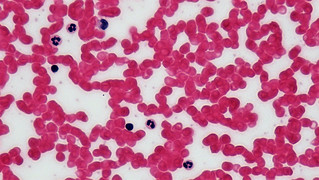
The manual technique of differential leukocyte count entails a visual examination of blood smear. A hemocytometer (counting chamber) can also be used for manual counting and entails direct counting of the cells in the inner squares.
Requirements
- Coplin jar
- Immersion oil
- Compound microscope
- Microscope glass slides
- Stain: Wright Satin
- 89% methanol
- Water
Procedure
· Place a drop of the blood sample on a clean microscope glass slide, and using another slide or coverslip at an angle, create a thin film.
· Allow the film to dry (air-dry) and dip in the stain for about 10 seconds.
· Dip the slide in water for about 20 seconds.
· Remove excess water and allow the slide to air dry then smear the immersion oil over the think film.
· Observe the slide under high magnification (X 1000) and study the distribution of the cells.
· Scan at least 10 fields in order to obtain more conclusive results.
Observation
· If there are between 0 and 2 cells per field of view, then the number of cells is low.
· If 3 to 6 cells are observed per field, then the number of cells is moderate.
· If more than 6 cells are identified per field of view, then the number of cells is high and maybe indicative of an infection.
Appearance
When viewed under the microscope:
· Lymphocytes can be identified by their dark-violet nucleus and characteristic blue cytoplasm.
· Monocytes can be identified by their lobed nucleus (medium purple in color) and blue cytoplasm.
· The nucleus of neutrophils will appear dark blue/purple in color with 3 or more lobes. The granules will appear red in color while the cytoplasm will be pink in color.
· Eosinophils can be identified by granules that appear reddish in color and a pinkish cytoplasm. The multilobed nucleus, on the other hand, will appear bluish in color.
· Lastly, basophils will contain purplish granules and bluish cytoplasm as well as a dark blue, bilobed nucleus.
Read about cell staining here.
Indepth look at Immunology as a field of study.
More on White Blood Cells here
Return from Leukocytes to MicroscopeMaster home
References
Ende Zhao et al. (2012). Bone marrow and the control of immunity. NCBI.
Choladda Vejabhuti Curry. (2015). Differential Blood Count. Medscape.
Cecilia Di Ruberto and Lorenzo Putzu. (2013). White Blood Cells Identification and Counting from Microscopic Blood Images. ResearchGate.
Lorenzo Putzu and Cecilia Di Ruberto. (2013). White Blood Cells Identification and
Classification from Leukemic Blood Image.
Z.H.Al-Zubaydi. (2011). White Blood Cells (WBCs) or Leukocytes. Medical Physiology.
Links
https://opentextbc.ca/anatomyandphysiology/chapter/18-4-leukocytes-and-platelets/
https://www.medicine.mcgill.ca/physio/vlab/bloodlab/WBC_count.htm
Find out how to advertise on MicroscopeMaster!
![Leukocytes, Illustration from Anatomy & Physiology, Connexions Web site.http://cnx.org/content/col11496/1.6/, Jun 19, 2013.by OpenStax College [CC BY 3.0 (https://creativecommons.org/licenses/by/3.0)] Leukocytes, Illustration from Anatomy & Physiology, Connexions Web site.http://cnx.org/content/col11496/1.6/, Jun 19, 2013.by OpenStax College [CC BY 3.0 (https://creativecommons.org/licenses/by/3.0)]](https://www.microscopemaster.com/images/512px-Leukocyte_Key.jpg)
![General pathology: Acute inflammation: Showing margination of neutrophils by Calicut Medical College [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)] General pathology: Acute inflammation: Showing margination of neutrophils by Calicut Medical College [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]](https://www.microscopemaster.com/images/Margination_of_neutrophils_in_acute_inflammation.jpg)