Where are Goblet Cells Located?
What are their Functions?
Overview: What are Goblet Cells?
Goblet cells are specialized secretory cells that line various mucosal surfaces.
They originate from pluripotent stem cells and are characterized by a cup-like/goblet morphology. Though they are primarily involved in the production of mucus, goblet cells also secrete a number of molecules such as chemokines that have been associated with innate immunity.
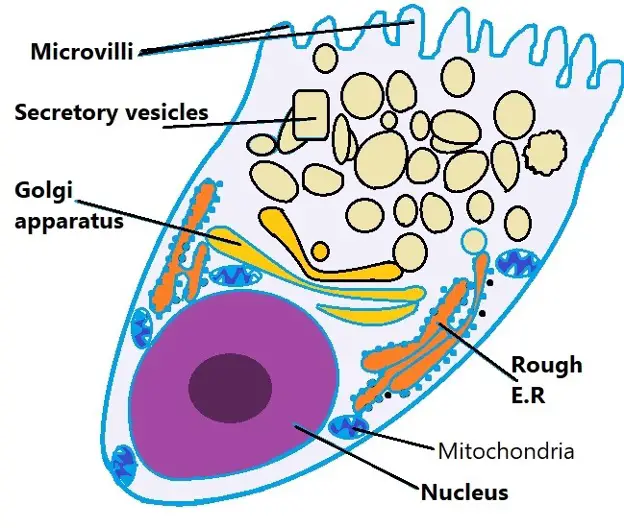
Diagrammatic representation of a goblet cell:
Goblet cells are characterized by a cup-like morphology. Many of the organelles, nucleus, mitochondria, rough endoplasmic reticulum, and Golgi apparatus, are located in the lower part of the cell (the basal portion) while the vesicles with mucins are located in the upper part of the cell (the apical part).
Where are Goblet Cells Located?
Goblet cells are largely found in the mucosal layer or epithelial layer of the gastrointestinal tract, the respiratory tract (upper and lower), as well as the reproductive tract.
In parts of the body like the airways (the epithelial surface lining the airways) the apical surface of the goblet cells protrudes into the surface which allows them to rapidly respond to changes (e.g. presence of foreign particles). In general, however, this ensures that the epithelia are continually covered with mucus for protection, by creating a physical barrier, while also keeping the tissues moist and lubricated.
* Goblet cells can also be found in the conjunctival epithelium.
In the intestinal epithelium, goblet cells are the most abundant secretory cells. Here, they are mainly involved in the production of trefoil factors (peptides that serve to protect and repair the epithelial surface) as well as mucin 2 (MUC2).
While goblet cells can be found along the gastrointestinal tract, they are particularly more abundant along the small intestine to the distal colon. However, the amount of mucus produced in the colon is more (two layers of mucous gel) than the amount produced in the small intestine (a single layer).
In the respiratory tract, goblet cells, among other types of cells, can be found in the tracheobronchial epithelium. They are largely involved in the production of mucins MUC51C and MUC5B. The mucins then combine with a number of other molecules to form a protective viscous medium layer that traps and helps in the removal of foreign and harmful particles and pathogens.
* Some of the cells that can differentiate into goblet cells in the gastrointestinal tract include basal cells and club cells.
Goblet cells can also be found in the epithelial lining of the eyelid (the inner surface). Here, goblet cells can be found in the fornix (a loose soft tissue) as well as the palpebral.
In addition to aqueous mucin (MUC5AC), these goblet cells also secrete components required for the production of trefoil factors, defensin, and peroxidase.
* Goblet cells are often described as being merocrine exocrine glands. As such, they release their secretions (packaged within vesicles) directly onto the surface of the epithelium.
What are the Functions of Goblet cells?
Mucus Production
Goblet cells are mainly involved in the production of mucus.
Increased secretion of this substance may be triggered by a variety of irritants (e.g. dust and smoke, etc.) along various epithelia. This type of secretion is known as stimulated secretion and is regulated.
In stimulated secretion, increased exocytosis of mucus granules is initiated by various extracellular stimuli. This allows for an appropriate response to the stimuli through increased secretion.
While goblet cells can be stimulated to produce high amounts of mucus, it's worth noting that these cells continually produce a low level of this substance through a pathway known as constitutive secretion (basal secretion). This pathway is unregulated and serves to protect and lubricate various epithelia.
* Generally, mucus consists of the glycoprotein mucin, water, and inorganic salts.
* In the stomach, the mucus (gastric mucus) is produced by secretory cells known as foveolar cells. Here, the mucus produced helps protect the stomach lining from the corrosive gastric acid.
Functions of Goblet Cells in the Gut
Lubrication
As mentioned, goblet cells can be found in the epithelium of the small intestine. Here, they help lubricate luminal contents which in turn allows for easier passage of food material along the tract.
Protecting the intestinal epithelium
The gastrointestinal tract contains a number of microorganisms (microbiota) particularly from the phyla Firmicutes and Bacteroidetes.
While many of these bacteria are not harmful, some can become pathogenic under given conditions. Strict pathogenic strains can find their way into the gut and cause serious infections.
In the absence of a mucosal barrier in this region, some of these bacteria can get in contact with the intestinal epithelium and easily cause an infection. Moreover, the infection can spread from this region to other parts of the body if the bacteria migrate between the epithelial cells to reach underlying tissues and organs.
Here, however, the mucosal layer acts as a barrier that separates these bacteria from the epithelia thus reducing the chances of an infection.
With a thickness of between 300 and 700 um, this layer, formed on the surface of the intestinal epithelium, forms an effective barrier that hinders the penetration of different types of microorganisms found in the gut.
Transmembrane mucins such as MUC3 and MUC13, etc. have been shown to cover apical surfaces of enterocytes with a structure known as glycocalyx. With a thickness of between 30 and 500 nm, this layer also acts as a barrier against microorganisms.
In addition to acting as a barrier, the mucus layer also helps remove trapped microorganisms from the lumen of the small intestine. In this case, old layers are removed along with trapped microorganisms while the layer is continually updated.
As already mentioned, goblet cells continually produce a given amount of mucus in order to maintain the barrier. This is especially important in that it prevents an accumulation of pathogenic substances and microbes.
* In mice, the absence of mucin protein has been shown to result in colitis. This is because bacteria (commensal bacteria) are easily capable of coming in contact with the epithelium and causing an infection. As well, human patients with an abnormally thin mucus layer have also been shown to be more susceptible to ulcerative colitis.
* The mucin can also immobilize some bacteria and prevent them from coming in contact with the epithelium. Based on a number of studies, adhesins used by bacteria for attachment and locomotion bind to oligosaccharide side chains located on the mucins which immobilize the organism. This also helps trap the pathogens making it easy for them to be eliminated as new mucus is produced.
* Aside from bacteria, goblet cells also produce mucin in response to a number of other parasitic infections. For instance, in some animals, hyperplasia of goblet cells has been reported in response to such worms as Ascaris galii and Trichuris muris in the gut.
A good example of this is the upregulation of Muc2 and Muc3 genes in mice following a T. spiralis infection.
Some of the other parasites that activate increased production of mucus include:
Immune Functions
Some immune functions of the goblet cells involve antigen sampling and tolerance.
Goblet cells have been shown to move some antigens to dendritic cells through a process known as transcytosis. Here, the antigens are taken into the cell through endocytosis before being transported to the underlying dendritic cells (within vesicles).
In this case, the goblet cell itself serves to move to transport the antigen (antigens of pathogen or foreign/harmful material). This results in the production of Immunoglobulin A (IgA) and consequently increased production of regulatory T cells.
Aside from influencing the production of regulatory T cells, goblet cells can also suppress inflammatory responses. Mucin 2 (MUC2 produced by goblet cells) stimulated AKT and GSK3β thus contributing to the inhibition of b-catenin. This activated increases transcription of tolerogenic cytokines.
* Oral tolerance - As with breathing, the ingestion of various materials (foods and drinks, etc.) introduces different types of antigens into the body. For this reason, it would be expected that the immune system would respond appropriately.
For the most part, oral tolerance prevents this response through the actions of goblet cells. Here, mucin produced by these cells acts on dendritic cells causing them to become more tolerant to these antigens.
Airway Goblet Cells
In the respiratory tract (airways), goblet cells are also located in the epithelium. Here, their apical surfaces protrude into the lumen. This allows them to rapidly respond to various changes as air is inhaled into the lungs.
Some of the irritants that induce increased goblet cell secretion include gases, inflammatory mediators, some changes in the environment, proteinases and neural agents, etc.
In human beings, the mucin produced by airway goblet cells is known as Mucin 5AC (MUC5AC). However, another type of mucin (MUC5B) is also produced by other surface secretory cells and submucosal glands found in this region.
The amount of each type of mucin produced is largely dependent on the type of irritant. For instance, the production of MUC5AC increases by 40 to 200 times in the event of allergic mucous metaplasia while MUC5B remains at the baseline level.
In mice, the production of Muc5b may increase 3 to 10 times in the event of allergic inflammation. Some of the other factors that may activate increased production of MUC5AC include viruses and acrolein.
The mucus gel produced in the airways is particularly important given that the respiratory system is exposed to a wide variety of foreign material and pathogens that are inhaled during breathing. The mucus layer is generally located above the periciliary layer.
The beating action of cilia easily propels the layer/gel in the proximal direction so that trapped particles, pathogens, and chemicals can be easily cleared. Like in the gut, mucins are continually produced in the airway in order to sustain the layer.
The rate at which mucin is synthesized, secreted, and cleared is influenced by the type of foreign particles and pathogens that enter the airways.
* Along with the beating action of cilia, coughing also aids in the expulsion of mucus (and trapped material/pathogens).
* In the eyes (conjunctiva), goblet cells produce mucins that help lubricate the ocular surface. Here, a reduced number of goblet cells, as well as increased cytokines, has been associated with dry eye disease.
Pathophysiology
Goblet cells have been associated with a number of diseases that may result from the overproduction of mucus or depleted number of the Goblet cells themselves. As well, their activities can help diagnose various conditions.
- Hyperplasia - As mentioned, with respect to goblet cells, hyperplasia refers to the increased or exaggerated production of goblet cells. Under certain conditions, increased secretion of mucus due to excessive proliferation of goblet cells is an indication of lung conditions like asthma. Goblet cells also may accumulate in the airways (metaplasia) resulting in excessive production of mucus. Rather than helping to trap and eliminate foreign particles and pathogens, they may end up blocking the underlying epithelial cells among other cells as well as the airway. This not only affects the normal functioning of the underlying cells but also results in long-term or chronic lung disease.
- Inflammatory disease - A number of chronic infections and parasitic intestinal infections have been shown to contribute to the depletion of goblet cells. In turn, this may result in the development of bowel inflammatory diseases like ulcerative colitis and Crohn's disease. In the small intestine and colon, goblet cells play an important role in producing mucus that prevents various pathogens and foreign material from coming into contact with the underlying epithelia. However, in cases where the goblet cells are depleted, mucus production significantly declines or ceases. This exposes the underlying tissue to a variety of pathogens and harmful components that can cause inflammatory diseases.
* Under normal circumstances, the colon consists of two layers of mucus. Here, the outer layer serves as a habitat for commensal flora while the inner layer (about 50 um thick in mice) helps prevent bacteria from penetrating and reaching the underlying epithelial surface.
Return From "Goblet Cells and their Functions" to MicroscopeMaster home
References
Heather Mccauley and Géraldine Guasch. (2015). Three cheers for the goblet cell: maintaining
homeostasis in mucosal epithelia.
Janice J. Kim and Waliul I. Khan. (2013). Goblet Cells and Mucins: Role in Innate Defense in Enteric Infections.
Kathryn A. Knoop and Rodney D. Newberry. (2018). Goblet cells: multifaceted players in immunity at mucosal surfaces.
Leticia Tordesillas and M. Cecilia Berin. (2019). Mechanisms of oral tolerance.
Links
https://www.physio-pedia.com/Goblet_Cells
https://www.sciencedirect.com/topics/neuroscience/goblet-cell
Find out how to advertise on MicroscopeMaster!