Mast Cells
Definition, Histamine/Inflammation, Vs Basophils
Definition: What are Mast Cells?
Mast cells are a type of white cell that resemble basophils (at least with regards to cytoplasmic granules) - as described in 1878 by the Nobel prize-winning German-Jewish Physician, Paul Ehrlich.
As compared to other white cells, mast cells are long-lived cells that can survive for several months (2- 3 months).
In addition to being widely distributed in the boundaries between body tissues and the external environments (in various connective tissues and mucosal layers) these cells also have a number of characteristics that enable them to act as first responders in certain circumstances.
They are capable of communicating with other immune cells thereby mediating the appropriate immune response. For this reason, they play an important role in both innate and adaptive immunity in the body.
* One of their other significant roles is their involvement in allergic reactions.
* Because of where they are located, mast cells have also been described as sentinels of the immune system or resident cells.
Mast cells can be found in the following areas:
- Near the blood and lymphatic vessels
- Bronchial epithelium
- Mucosal surfaces of lungs and gut
- In the skin
Origin and Development of Mast Cells
Mast cells arise from the monopotent mast cell progenitors (CD34+ pluripotent stem cells) located in the bone marrow and the intestine through a process that is regulated by transcription factors.
Unlike some of the other white cells, however, these cells are released into the bloodstream in the form of mast cell progenitors (MCp). It's when these immature cells reach the peripheral tissue that they begin to mature.
In the peripheral tissue, the migration of mast cells is regulated by a number of processes that are stimulated by inflammation. Therefore, from blood, mast cell progenitors are recruited in cases of inflammation which influences terminal differentiation allowing them to act accordingly.
* Some of the mast cells in peripheral tissue are difficult to identify because they lack granules.
Some of the characteristics of mast cells include:
- They are mononuclear cells - They have a single, intact round nucleus
- Small secretory granules that range between 0.2 and 0.8 UM in diameter
- They are coated with IgE receptors
* The density of mast cell granules may obscure the nucleus.
Inflammation
The role of mast cells in inflammation:
Allergic Inflammation
Mast cells are heavily involved in the pathophysiology of such allergic diseases like allergic rhinitis, dermatitis, and asthma. In particular, these cells are involved in hypersensitivity reactions mediated by IgE (Immunoglobulin E).
Upon activation by an allergen (mites, dust, and pollen in the case of asthma) mast cells release various mediators into the environment. These may include such mediators as histamine, chemokine ligand 2 and tryptase that in turn impact the tissue around them.
Upon release, these mediators may result in increased permeability of the epithelium, high production of mucus production, vasodilation of the blood vessels as well as contraction of the smooth muscle.
In turn, this helps recruit such cells as basophils and neutrophils that actively destroy the foreign material in the affected site.
Role of Inflammation Mediators: Histamine
Inflammatory mediators (eicosanoids, histamine, and cytokines, etc) play a crucial role in allergic diseases. Histamine is one of the most important mediators and is found in high concentration in the skin, intestinal mucosa and the bronchial tissue where it serves to stimulate the development of allergic-related inflammatory reactions through the regulation of the appropriate white cells.
Here, however, it is worth noting that in an allergic inflammation, histamine can have pro-inflammatory or anti-inflammatory effects. The final outcome is dependent on the subtype of the receptor of the histamine as well as the type of cell being stimulated.
Whereas the HI-receptor is involved in such activities as vasodilation, cellular migration, and bronchoconstriction, etc, the H2-receptor is largely involved in such events as vascular permeability and the production of airway mucus.
Some of the other histamine receptors include:
- H3
- H4
- H4R
Role of Mast Cells (and Histamine) in Allergic Rhinitis
Allergic rhinitis/hay fever is a type of inflammation caused by an overreaction to allergens present in the air. As such, it is a good example that can help understand the role of mast cells in allergic inflammation.
As a result of exposure to an allergen, mast cells are recruited to migrate and proliferate in the epithelium of the nasal cavity. This is caused by Chemokine (C-C motif) ligand 5 (CCL5) which is a chemoattractant that is found in high concentration in the nasal epithelium.
In the epithelium, degranulation of mast cell results in the release of histamine, tryptase, and LTC4 among others. In individuals with allergic rhinitis, these molecules (mediators) have been shown to be elevated thus signaling the degranulation of mast cells.
The release of these molecules is associated with such events as pruritus, nasal congestion and sneezing among others. Here, histamine has been shown to be largely involved in vasodilation, high glandular secretion as well as vasodilation.
By acting on the nerve endings of sensory neurons, histamine also causes sneezing experiences in allergic rhinitis. Through further activities of mast cells and histamine, eosionophillic infiltration follows.
* Degranulation in mast cells is stimulated by the binding of antigen to the immunoglobulin E antibody present on the surface of the cells. This process is characterized by the release of mast cell granules which are rich in such molecules as histamine and heparin.
Non-Allergic Mast Cell Activation
While mast cells have been shown to be actively involved in allergic inflammatory reactions, studies have also shown that non-allergic components also have the capacity to activate mast cells in the absence of IgE. In this case, the inflammation may also be observed even in individuals who do not suffer from such allergic reactions as asthma or allergic rhinitis.
* Mast cells cause inflammation through such neutrophil chemoattractants as interleukin 8 and tumor necrosis factor-α (which are released immediately the cell is activated) or through the release of such molecules as histamine and serotonin that not only affects the structure of their surroundings (e.g. increased vascular permeability and fluid influx) but also promotes the migration of immune cells to the affected site.
Role of Mast Cells in Innate and Adaptive Immunity
Innate and adaptive types of immunity help protect the host against different types of infections. Whereas the first line of defense (innate immunity) is naturally present in the body and fights any invader, adaptive immunity has to be created in response to the presence of foreign invaders.
It acts against specific infections in the body. Because of their unique localization, they are involved in both types of immunity.
As already mentioned, mast cells are typically located in the boundaries between body tissues and the external environment. This is of great significance in innate immunity given that these are the common sites of pathogen invasion.
As a result, they are well positioned to provide the first line of defence against a variety of pathogens. In one study, parasitic infection of the intestine was associated with high levels of mast cells (hyperplasia) as well as the release of proteases that ultimately eliminated the parasites. Here, then, through the disruption of the intestinal epithelial barrier, mast cells were shown to play an active role in innate immunity.
Against bacteria, mast cells have been shown to play a role in innate immunity through:
- Bacterial phagocytosis
- Processing and presenting bacterial antigens to the appropriate immune cells
- The recruitment of other phagocytic cells
- The release of appropriate mediators
- Production of antimicrobial peptides that act on the invader
By recognizing specific structures on the surface of invaders (e.g. recognition of FimH present on the surface of E. coli). This identification allows the cells to bind and phagocytose bacteria.
Apart from binding and phagocytosis action of mast cells, mast cells have also been shown to be capable of expressing TLRs, a cell-surface receptor that not only binds to specific molecules on the microbe, but also stimulates the production of pro-inflammatory cytokine which in turn helps in the elimination of the invading microbes.
Mast cells have been shown to play a role in innate immunity against a number of intracellular parasites.
Some examples of these parasites include:
- Malaria parasites
- Toxoplasma gondii
- Giardia lambria
- E. coli
- M. pneumoniae
- Trypanosoma brucei
Adaptive Immunity
For the most part, the role of mast cells in adaptive immunity has been shown to be in relation to T lymphocytes. This, for mast cells, is made possible by the ability of the cells to serve as antigen-presenting cells.
In response to certain infections, mast cells have been shown to migrate into the lymph nodes and produce cytokines and chemokines that not only induce hypertrophy of the lymph nodes, but also cause aggregation of lymphocytes.
Here, cytokines have also been shown to induce the differentiation of T helper 2 (TH2) cells which in turn elevates an allergic immune response. Through the secretion of IL-12 and INFγ, mast cells are also capable of enhancing the response of TH1 and thus ensuring equilibrium between the response of T helper 1 cells and T helper 2 cells.
Apart from inducing the recruitment of T lymphocytes, mast cells also regulate these lymphocytes during an immune response by modulating dendritic cells. In addition, they have a regulatory effect on B cells and thus on their actions.
It's worth noting that both B and T lymphocytes are cells of the adaptive immunity system.
They have the following three primary traits:
· Specificity - they can recognize certain antigens and respond in a specific manner
· Memory - They can retain information regarding a specific antigen and thus act rapidly when they come in contact with the antigen for the second time
· Self-Recognition - This allows them to destroy cells that are no longer recognized as self (due to occurring changes)
Mast Cells Vs Basophils
Both mast cells and basophils share a number of characteristics in relation to their function and development. At the same time, they also have a number of differences that will be discussed in this section.
Like mast cells, basophils are also involved in various allergic and inflammatory diseases. This is because the two produce high amounts of mediators like histamine that play a central role in inflammatory responses.
The two have been shown to share a number of features such as metachromatic granules and high-affinity receptors that enable them to identify and mount a response against invading organisms (bacteria and multicellular parasites like helminths).
Like mast cells, basophils are also referred to as effector cells. As such, they are capable of producing various bioactive molecules (e.g. cytokines, proteases, and chemokines etc.).
These molecules are actively involved in several processes that are directed towards protecting the host. For instance, histamine and cytokines play an important role in inflammation responses as well as in reactions against infections brought about by parasites,
While mast cells and basophils share a number of features, differences between the two are evident in their respective life span, where they are located in the body as well as proliferation.
As previously mentioned, mast cells arise from the bone marrow and are released into the bloodstream as immature cells only to mature in peripheral tissue. This is different from basophils that mature in the bone marrow and circulate in peripheral blood as mature cells.
Unlike mast cells, which are long-lived, the life span of basophils is significantly shorter given that they can only survive for a few days (about 3 days compared to mast cells that can survive for a few months).
This characteristic of basophils may be attributed to the fact that they do not proliferate once they mature. While mast cells only differentiate in tissue, they are capable of proliferating in these sites and therefore continue renewing themselves.
Microscopy and Histology of Mast Cells
Some of the histochemical methods used for staining mast cells include:
- Luna stain
- Sudan Black B
- Ziehl Neelsen
- Toluidine blue
This section will focus on Toluidine blue staining protocol
Requirements
- Tissue sample (paraffin section)
- Toluidine blue stain
- Distilled water
- 95 and 100 percent alcohol
- Microscope coverslip
- Xylene
Procedure
- Using distilled water, deparaffinize and hydrate the tissue sections
- Stain the section using Toluidine blue for about 3 minutes
- Wash the sample using distilled - repeat this three times while changing the water
- Dehydrate the sample using 95 percent alcohol (two dips)
- Dehydrate the sample again using 100 percent alcohol (several dips)
- Clear using xylene
- Cover the sample/section with a coverslip (a resinous mounting medium may be used to keep the coverslip in place)
- View under the microscope
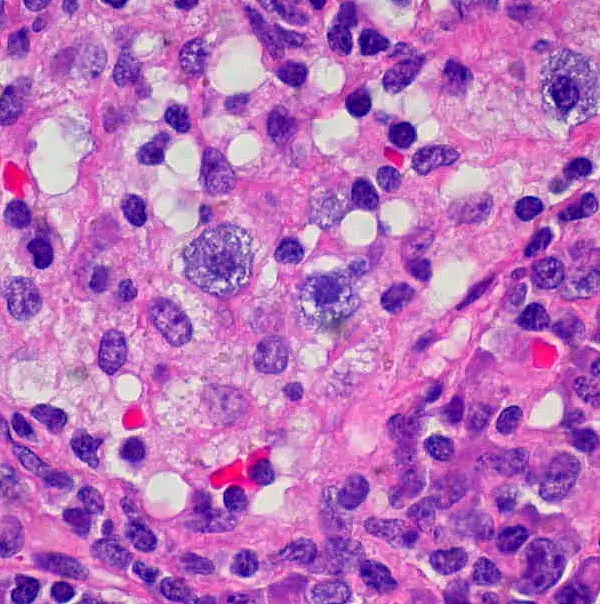
Observation
- When viewed under the microscope, mast cells will appear violet or purple in color
- Granules are easily recognized (violet or purple in color )
Image below of mast cells under the microscope: Toluidine blue staining
Of interest: Bacteria under the Microscope
Return to White Blood Cells main page
Return to Red Blood Cells main page
Return from Mast Cells to MicroscopeMaster home
References
Adaya Weissler Snir and Yoseph A Mekori. (2009). The Role of Mast Cells in Non-Allergic Inflammation. ResearchGate.
Domenico Ribatti. (2018). The Staining of Mast Cells: A Historical Overview. Experimental Allergy – Review Article.
Kawa Amin. (2012). The role of mast cells in allergic inflammation. Respiratory Medicine.
Michael Fong and Jonathan S. Crane. (2018). Histology, Mast Cells. NCBI.
Martin Metz et al. (2011). Evidence for Non-Allergic Mast Cell Activation in Pollen-Associated
Inflammation. ResearchGate.
TC Moon. (2009). Advances in mast cell biology: new understanding of heterogeneity and function. Nature Publishing Group.
Thomas J. Palker, Gang Dong and Wolfgang W. Leitner. (2010). Mast cells in innate and adaptive immunity to infection. Eur. J. Immunol. 2010. 40: 13–18.
Zhenping Wang and Anna Di Nardo. (2011). Sentinel Role of Mast Cells in Innate Immunity. ResearchGate.
Links
https://www.immunology.org/public-information/bitesized-immunology/cells/mast-cells
https://link.springer.com/article/10.1007/s00281-016-0582-0
Find out how to advertise on MicroscopeMaster!
![Mast cell contain histamine,other inflammatory mediators & heparin.Special stain used for is Toluidine blue by Dr. Roshan Nasimudeen [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)] Mast cell contain histamine,other inflammatory mediators & heparin.Special stain used for is Toluidine blue by Dr. Roshan Nasimudeen [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)]](https://www.microscopemaster.com/images/Mast_cell.jpg)




